Have You Been Getting the Right Treatment? 11 Recommended Steps for High Quality Care
At the Consortium Physiotherapy Clinic Hull we see regularly see a large volume of patients complaining of back pain, neck pain, shoulder problems and knee issues.
Published in the British Journal of Sports medicine this year was a systematic review (source) of 44 best clinical practice guidelines. They highlighted huge gaps between what the growing body of research and evidence says we should do and what is actually provided in many clinics.
11 recommended key points
1. Care should always focus around YOU the patient
2. Your clinician should always screen you and try to rule out serious and sinister conditions
3. You should also be assessed for a variety of cognitive, social, lifestyle and emotional factors that are likely to influence your care
4. Imaging should not be routinely used unless you are suspecting serious pathology, have failed treatment and/or your symptoms are progressing and are hard to explain
5. You should be physically examined which may include neurological screening tests, functional tasks, flexibility and/or muscle strength
6. Your progress should be measured using tools called outcome measures which are often questionnaires that assess your musculoskeletal health
7. Education about your condition and the options open to you to help manage it is essential
8. Participation in physical activity and/or exercise should form a key part of your management plan
9. Passive treatments where you are mobilised, massaged or manipulated should only be used alongside other evidence-based treatments, this type of treatment should not make up the majority of your care
10. You should always be offered evidence based conservative management before being referred for a surgical opinion or considering surgery
11. Where possible we should help your either continue to work or assist you in getting you back to work
The Ten Benefits of Massage Therapy & Sports Massage
So you have back pain - do you actually need a MRI?
This video is another fantastic resource and an absolute must see for any patient with lower back pain
It provides some good examples of where a MRI scan is needed and where, as in many cases, it can distract you from getting better
Should you present to us with symptoms that require a MRI scan to be performed, then this is something we can arrange for you quickly and have it reviewed by our spinal surgeon
If a scan is not be needed then we can focus immediately on the most important thing, getting you better
Thanks for reading
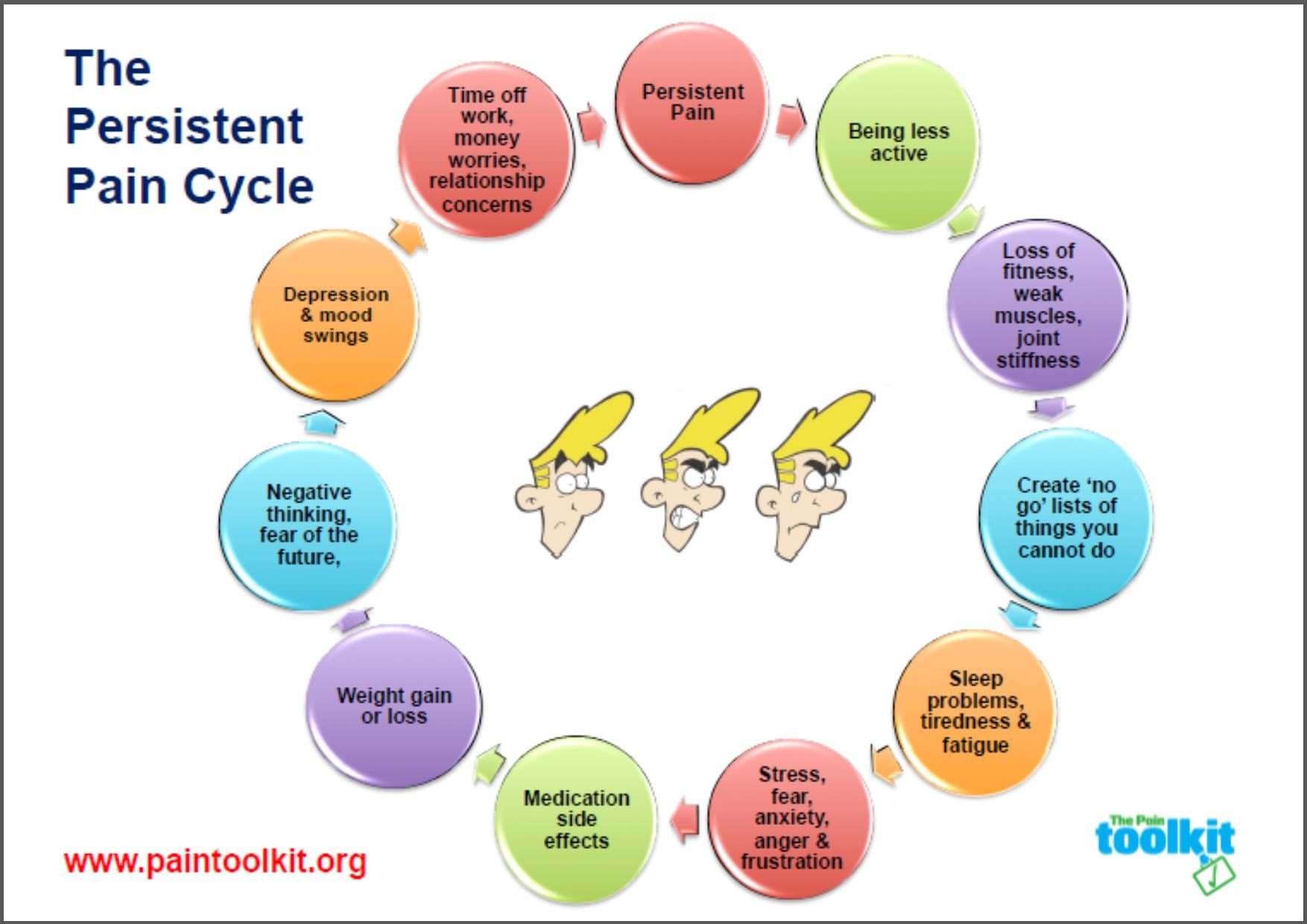
Chronic pain cycle
This diagram will be familiar territory for many people living with pain. We encounter patients on a daily basis who are stuck in this cycle...
TRYING TO EXERCISE BUT YOU CAN’T BECAUSE OF PAIN? LEADING TO MORE WEIGHT GAIN, MORE TISSUE DECONDITIONING, MORE TIME OFF WORK, MORE STRESS, MORE SLEEPLESS NIGHTS, MORE DEPRESSION, MORE PAIN…
Diagram reproduced with permission from Pete Moore/paintoolkit.org
In many patients this cycle can be minimised to varying degrees. Consortium provides physiotherapy including: pacing, CBT (Cognitive Behavioural Therapy), acupuncture, TENS therapy, education, sensibly prescribed simple and graded exercises, medications, injections and manual therapy. These are all valid ways to intervene. Alongside this we offer support, encouraging patients to reach acceptance. Many of these can be easily implemented in simple ways, without significant costs.
There are many free, easily accessible resources available for patients living with pain. Here are two that we often direct people towards:
LEAFLET explain pain - click here
video understanding PAIn in less than 5 minutes
Thanks for reading
Tissue Regulation
Perhaps the best way to introduce this topic would be to pose the following questions..
Why do some runners demonstrate a poor style with limbs thrown all over the place with no obvious control yet they can continue uninjured?
So how are these lucky individuals able to continue to exercise pain free while many people with better style and form continually run into strings of injuries?
It seems clear therefore that injury does not solely relate to style, biomechanics or perfect alignment.
Each of us has a certain amount of capacity in our tissues to tolerate stresses and loads. Some may have a huge amount of leeway (the sloppy runner who is injury free) and others very little (the perfect runner who is always injured). Some people may be able to suddenly and drastically increase their training loads without injury, while others only have to make the most minimal of changes and they run into trouble. As a general rule of thumb however large changes in activity does seem to be a precursor to injury. The concept of tissue regulation and capabilities of tissues to tolerate load is not something new, in fact it was first described by Scott Dye an American knee surgeon in 2005 (Source).
The model that Scott puts forward should have huge influence in the way we treat patients today. We feel this is a very important concept for the majority of our patients to understand and we have tried to explain it in its most simple terms.
OPTIMAL LOADING - sensible appropriate loads at the right intensity, speed and position with the correct amount of recovery will in time improve the capability of that tissue to tolerate load. No different from training for a marathon, take it too quick and you run the risk of injury, take it too slow and you waste time. It is a balancing act.
UNDERLOADING/SUBOPTIMAL - e.g complete rest! This will create the reverse effect and decrease the tissues capability to deal with load, as it would when you take time out injured. This can result in malnourishment, pain and pathology. The same principle applies with overloading. This is why we will try to avoid at all costs and will very rarely prevent you from having to stop participating in your activity.
How do you know if your exercises are pitched into the right zone for you?
If you can tolerate your current exercises/training load or activity in a pain free manner, with no flare up of pain on the second day after exercise then you are likely to be working within a capable zone for that tissue. Be careful though as it is common for tissues to flare up 24 hours later. This can often be due to a latent production of an inflammatory chemical called cytokines.
No pain, no gain in the majority of cases is therefore not applicable what so ever!
What is the ideal?
Theoretically it is best to remain working at the upper limit of your optimal zone. Loading OPTIMALLY and allowing correct progression and recovery time will increase the capability of that tissue to deal with a task in a healthy manner.
What to do if I'm injured?
You will need to work in a lesser zone and then slowly build back up again. Even injured joints can function very well with certain activities. Examples of this can be using swimming and cycling where there is less direct impact yet you can still maintain strength and movement without continuing to overload and worsen your injury.
In summary, your tissues don't take well to sudden changes. Changes such as increases in training need careful grading. Think of your tissues like employees, if you drastically change someone's job role overnight without prior warning, you will have outrage and backlash on your hands. If you make small changes and are appropriately prepared it will make for a smoother transition. This is an especially important principle when dealing with patients chronic pain, they may well need to take much smaller steps and take them over a much longer period of time.
Exercise prescription is therefore something that should be taken extremely seriously. It is not just a case of picking exercises, giving them a go and quickly abandoning them if they don't give you the results you want. Exercises and training regimes must consist of OPTIMAL loads and need to be sensibly and accurately applied. The volume and intensity of your exercises needs to be monitored in order to be able to progress and regress them appropriately. The principles we have discussed here about regulating tissues must be applied in order to ensure successful recovery.
Thanks for reading
Are you a victim of misleading medical imaging?
It is only natural if you have a problem to want to resort to some form of imaging to try to identify a cause. From a patients perspective this is understandable, for patients, it makes logical sense. Unfortunately, as with most things there is far more to consider here as we will go on to explain... Patients are misled by imaging so frequently that we feel it is very important to cover this topic early on.
ARE SCANS USEFUL?
Absolutely this is a yes, they are key to many things. This is not a one sided argument about the problems we encounter with misleading images however. Obviously scans are essential for surgical planning, identifying major/serious pathology, fractures, lesions and dislocations etc.
Will my scan ACCURATELY identify my problem?
It is very common for scans to show abnormalities that do not relate to a person's symptoms. These findings are often purely radiological incidental findings! Our clinicians interpret images in daily surgical clinics and constantly encounter these issues when analysing the hundreds of MRI and Ultrasound scans we come across a year. We find ourselves often explaining to patients why it is that their MRI scan shows a huge disc prolapse clearly compressing a nerve on the right side but yet their symptoms are only on the left!
FACTS AND FIGURES
SPINAL MRIS
48% of 20-22 year olds with absolutely no back pain or any issues had at least one degenerative disc seen on their scan, at least 25% had a disc bulge showing. (Source)
40% of individuals under the age of 30 and 90% of people over the age of 50 have disc degeneration, yet they are pain free. (Source)
One study found 98% of men and women with no neck pain had degenerative changes seen on their MRI scan. (Source)
SHOULDER ULTRASOUND SCANS
20% of pain free adults had a partial rotator cuff tear on MRI scan with 15% showing a major full thickness tear! For those people over 60, at least half have a rotator cuff tear they never even knew about. (Source)
KNEE XRAYS
If you x-ray a normal population of adults with no actual knee pain, at least 85% of the x-rays taken will show arthritis. (Source)
In one study, 48% of professional basketball players were shown to have cartilage damage on their knee MRI scans, none had any pain. (Source)
WHAT DO WE TAKE FROM THIS?
Degenerative changes are simply normal. What we see on our scans, often does not represent reality. There is no need to worry if your scan shows certain changes, they are not necessarily associated with pain. If you allow your images to mislead you, theoretically you could end up in higher amounts of pain for longer amounts of time.
Don't get us wrong, as previously mentioned, where appropriate, imaging is an important part of a patients care. Our clinicians at consortium rely upon images to make surgical decisions in conjunction with the surgeons we work with. What is essential is that a patients symptoms directly correlate with the symptoms that they present with. Both us, and patients need to make sure we do not get side tracked with purely incidental findings. Next time you somebody tells you that your discs are worn out or your shoulder is torn then I hope you can see there is no reason to immediately panic! It is absolutely feasible for patients with worn out joints to function at high levels with no symptoms.
Thanks
The Consortium Team
Hello! Welcome to our blog...
So this is our first ever blog as Consortium physiotherapists. We have known for a long time that we wanted to open this clinic and have spent a lot of hours discussing the ideas and principles behind our service.
We want to provide a forward thinking evidence based approach in a completely open and honest way. We are passionate about our profession and believe that we can provide a huge amount of expertise to boost the quality of care in our regions private physiotherapy sector. It is important to us to empower our patients, promote activity and avoid using the long established passive treatments that unfortunately still haunt many private physiotherapy practices across the uk.
We want to utilise this blog as a way to educate our patients about recent developments within our field. We will be including posts that focus on providing valuable advice and information, dispelling many of the traditional myths that we find are still being fed to patients on a day to day basis.
We also want our customer experience at Consortium to be comfortable, convenient and enjoyable. For that reason we have spent a lot of hours considering how we want our clinic to look and feel inside. We are renovating what will be our clinic site as we speak and let's just say it has been a labour of love. Anyway, the diggers have now finally cleared out, the excavation is complete and we are starting to see some exciting progress! The building itself is a pretty old one, with a good amount of character so we intend to make the most of this and keep its style traditional but with a modern edge. Inside there will be two large private clinic rooms, a comfortable waiting area with reading material, TV and Wi-fi for customer use (some home comforts are always good).
Outside we have a large spacious private car park, accessed through a private gated entry for an easy parking experience. We hope to be ready to see patients early in 2016. There is quite a bit of extra land on site so once up and running we also plan to build a well equipped gym to aid aspects of our exercise therapy and movement analysis.
So that's an update on where we are at the moment with Consortium. Now that you know a bit about us as a group, next time we'll share a bit more about us as individuals and let you know what each of us will bring to the service. We hope you'll join us to read this from time to time and feel free to share your comments, they are always welcome.
Thanks,
The Consortium Team